In 2019, representatives from voice recognition software firm Nuance approached Queensland’s Mackay Base Hospital with a proposition. Nuance was offering 25 free licences to its new Dragon Medical One (DMO) product, which can integrate with the Cerner ieMR used in Queensland, to test it out to speed up clinical documentation.
Dragon voice recognition software has been used for well over a decade in healthcare – Northern Sydney LHD first trialled an integration with Cerner’s FirstNet and Dragon in Manly Hospital’s ED back in 2012, for instance – but the technology did require some training on the user’s voice and there were acknowledged problems with unfamiliar accents. It was good for dictation but required the use of a headset and almost invariably a medical transcriptionist to clean up the notes.
Dragon was and is widely used by specialist medical practices and is integrated in to practice management software, and its PowerScribe One is very popular with radiologists. Voice started to become far more attractive for acute care, however, when Nuance launched Dragon Medical One in 2018-19, moving it to the cloud and using infinitely more powerful AI. No longer did it need to be trained, the accuracy was much improved and clinicians could use it to speak directly into the EMR.
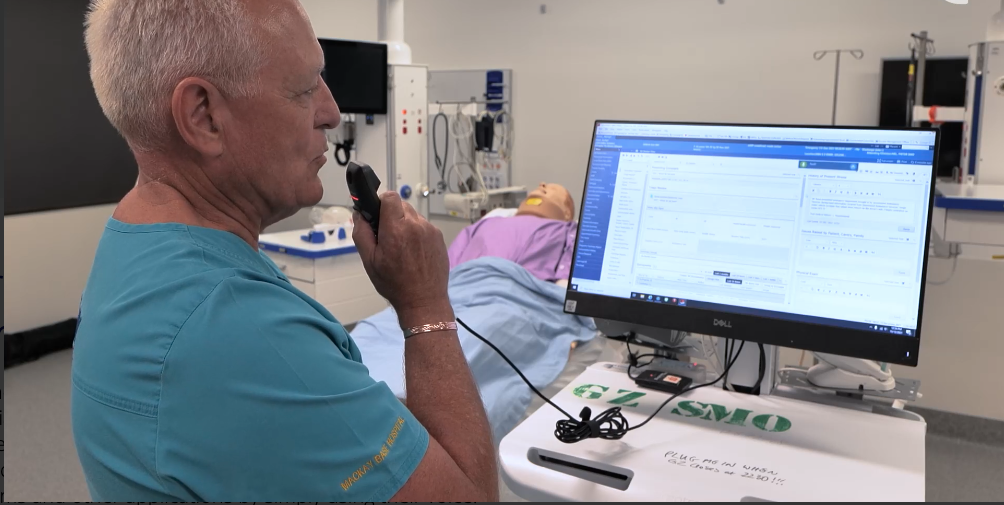
DMO is available to NSW Health clinicians who want to use it, and has now been pioneered in Queensland by Mackay HHS, where emergency department doctor, sometime GP and now chief digital director for medical services Pieter Nel has become a big champion of the technology following a successful trial in 2020.
Dr Nel spoke about the trial at MedInfo in July and is not afraid to say that he has gone from sceptic to salesman. He was immediately impressed with the ease with which it dealt with his South African accent, and the trial he and his colleagues ran saw the technology chosen for a wider rollout to rural sites in the HHS and shortly to other big health services in the state.
Voice has long been touted as being one answer to reducing the burden of onerous tasks in the EMR and it seems it is finally getting there. Mackay’s whole emergency department is using it, as is ICU and mental health, and Dr Nel is pleased to report that clinicians are saving time, money and their sanity by being able to go home from work on time.
Meanwhile, Nuance was further exploring the concepts of conversational AI and ambient clinical intelligence, which Microsoft was also working on with a view to reducing burnout problems due to burden of clinical documentation. The two worked together to develop Dragon Ambient eXperience (DAX), which Nuance hoped would do for patient consultations what DMO does for clinician interaction with the EMR. DAX brings voice recognition and generative AI to clinical documentation to capture natural conversations and put them in a complete clinical note.
Microsoft then put a price on the potential of the technology when it bought Nuance for $25 billion in 2021, but such is the speed at which AI is developing that it now plans to bring out DAX eXpress, which has integrated OpenAI’s GPT-4 multimodal large language model to promise a workflow-integrated, fully automated clinical documentation application that it says is the first to combine proven conversational and ambient AI with GPT-4.
Nuance says DAX Express will automatically and securely create draft clinical notes in seconds for immediate clinical review and completion after each patient visit in the exam room or via telehealth consults. It will be available to all Dragon users and integrated with DMO, and is EMR agnostic. Nuance is hoping to release the first iteration with Epic for general use in the new year.
According to Microsoft’s health industry executive for ANZ Simon Kos, Nuance is also working with Epic to use virtual assistants and ambient clinical documentation in Epic’s Haiku app for physicians to retrieve schedules, patient information, labs, meds and visit summaries, and for nurses to use voice-enabled workflows for documentation and flow sheets in Rover.
Back in Mackay, and Dr Nel is still singing DMO’s praises. New doctors will all be offered training in the technology when they start, and for senior doctors, Dr Nel believes there will be a reduction in burnout simply by relieving a lot of the documentation burden and allowing clinicians to go home on time.
Do you agree? That’s our poll question for this week:
Is AI the solution to EMR burnout?
Vote here or leave your comments below.
Last week we asked: Are NZ’s data and digital strategies ambitious enough? Our readers were split 50:50.
We also asked: If yes, is that because they were over-ambitious in the past? If no, what else needs to be done to accelerate digital adoption? Here’s what you said.





So, is AI the solution to EMR burnout? Again, it was a close-run thing: 57 per cent voted yes, with 43 per cent saying no.
We also asked: If yes, are you using AI for documentation now? If no, let us know why.
– No, still unreliable and must always check anyway
– A conditional ‘no’. If one reads the reviews and predictions for AI in health and the EMR there are significant positive and negatives. If looked at from clinicians burnout there is a strong possibility that the ‘seductive dependence’ on the AI technologies may allow errors e.g. of overuse, underuse and inappropriate use of health resources to be missed but more importantly the decision makers will become more seduced by the technology and lead to more ‘forgetting’ about the patient (Francois Gremy).
– AI can assist the clinical work, but the burnout is mainly caused by poorly designed the workflow and forms which cannot be solved by simple AI in text analysis.
– Not using as not integrated with GP software
– “AI” may possibly work for free text notes in general practice, but there are significant number of powerforms and power notes in powerChart for inpatients arising from the complexity of and standardisation of care efforts – i cannot see that “AI” can do any of that documentation work
– no not available yet. It is part of the solution only. Unrealistic workload expectations will remain an issue across health
– Using Fathom for webinar recordings
– It is no silver bullet, but it WILL help. Slow typists will be faster and more accurate, autofill lists will be enabled and a whole heap of other productivity aids will be realised through deploying DMO.
AI is only as good as the information we provide it, if the data isn’t there it will not make it up…well we don’t want it to.
We will need standards for the AI tools and training for our workforce, including me.