The federal budget handed down on Tuesday evening ticked a lot of boxes for the health and aged care sectors and was warmly welcomed by most, not the least by many aged care workers who will receive a decent wage at last. GPs seemed happy enough with the tripling of the bulk-billing incentive and the restoration of telehealth items for long consultations, tied as they are to voluntary patient enrolment.
The digital health sector did well enough too for those in favour of the My Health Record, which saw a substantial boost to normal funding to enable the Australian Digital Health Agency (ADHA) to put some serious effort into modernising it over the next two years. Normal operational funding for the system is usually about $150-160 million a year, but this year funding was up to $429m over two years.
When added to the substantial work the agency has already done on modernising the system – including moving the system to the Microsoft Azure secure public cloud and releasing the new Health API Gateway – the extra funding should see some serious improvements over the next two years.
ADHA could perhaps put a bit of work into publicising the my health app, released back in March. Everyone we’ve spoken to who has used the app is happy enough with it and we think it works really well. The agency says there are now 55,242 linked users of the app; we reckon this should be much higher given its ease of use. Perhaps a little old-fashioned ad campaign could kick it along a bit.
The funding for My Health Record was mainly welcomed by Pulse+IT readers if our poll from last week is anything to go by. Sixty-two per cent of readers said they were in favour of the pre-announced funding for system, while 38 per cent were not too keen. There were loads of comments on our poll: take a look here for a sample.
So funding for MyHR is secure for the next two years and ADHA has had its funding put on a more secure basis as an ongoing entity. You get the feeling though that Health Minister Mark Butler is keen to see some measurable results from the modernisation program. Meaningful use is back as a concept.
Also in the budget was $111.8 million over four years and $24.2 million in ongoing funding for the Department of Health and Aged Care’s electronic prescription delivery system overhaul. The reason behind the necessity for this program has always been a bit shrouded in mystery but with Fred IT not unexpectedly winning the tender and a mention that pharmacists will no longer have to reconcile every eScript dispensed with the eScript fee, it should all work a little more smoothly.
Mandating the use of the system for high-risk and high-cost medicines also makes sense. It also looks like the Medical Software Industry Association has got its way with the department allocating funding for prescribing and dispensing software vendors to remain compliant.
In other budget news, Western Australia has come through with funding for its electronic medical record program. We’re still a little hazy on what this actually means – WA did a request for information for am EMR a couple of years ago but has signalled in this budget that it intends to complete the roll-out of its DMR to hospitals not yet using it. The budget has funds for an ICU EMR for Perth Children’s and Charlies, neither of which use the DMR as far as we know, what this “EMR” consists of we’re not sure. We have a request in with WA Health for more information and will let you know when we hear back.
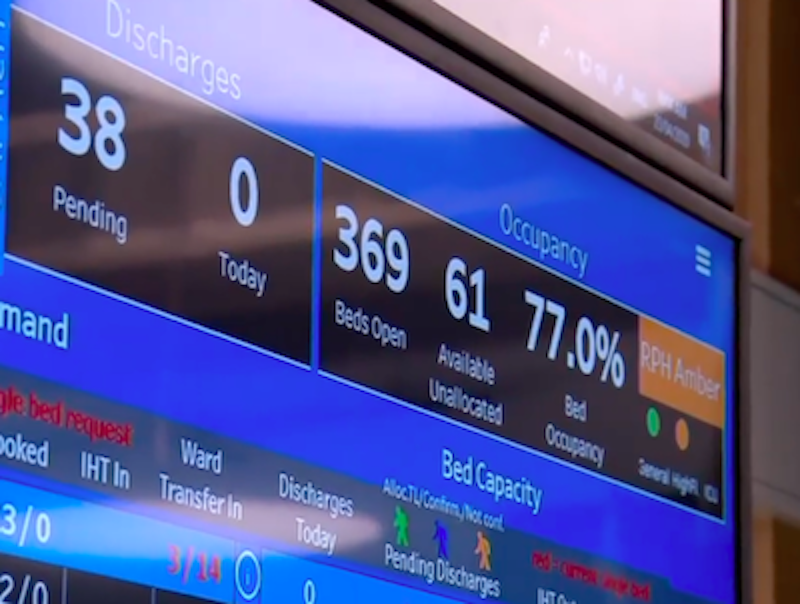
The WA budget also including funding for the roll out of the WA Virtual ED project, the State Health Operations Centre (SHOC) and for a smart referrals system. These projects are all part of a concerted effort to improve patient flow, reduce bed block and ramping and improve discharge times in Perth metro hospitals, all supported by the real-time demand data platform program.
There is loads of great technology out there to help with this sort of thing and we are very pleased to see WA Health put some money into it. The idea of a state operations centre is an excellent one for a state like WA, where critical care is concentrated in urban centres and a thriving rural virtual care service is already established. It gels with emerging ideas using command centres to provide oversight of hospital, district and statewide patient demand and flow, allied to patient-facing concepts like digital front doors. We’ll have two really interesting stories on these ideas next week, one from Queensland’s Healthcare Logic and another from global health IT firm Orion Health.
That brings us to our poll question for this week:
Is a State Health Operations Centre a good model for other jurisdictions?
Vote here, and leave your comments below.
As we mentioned above, in our last poll, 62 per cent said they were in favour of continued funding for the My Health Record,, while 38 per cent were against. Here’s what you said.
And finally, we were most pleased to see that Australasian Institute of Digital Health CEO Louise Schaper has scored a couple of big names to have a fireside chat with at the MedInfo conference in Sydney in July. Dr Schaper is a beacon of positivity and a terrific interviewer, so talks with Google’s chief health officer Karen DeSalvo and Oracle Health’s (Cerner) chairman David Feinberg will be something to look out for.
Yes, IF they are linked well to other services. We ran a VED and showed that many patients could be served in other ways without an ED, however, they need an alternative e.g. a nurse to go out, a physio etc. Provided it is connected well to provide this, I’m for it. Without that it does not have as good value.
Is a State Health Operations Centre a good model for other jurisdictions? Most said yes: 67 per cent were in favour, 33 per cent were against.
We also asked: If yes, why? If not, where else should the money be spent? Here’s what you said.
– Another bureaucratic layer
– Appears to be another layer of bureaucracy. One thing the system isn’t capable of is keeping things simple. The EMR’s that exist in this country are a perfect example of failure on a mega scale. Simple isn’t easy to do which, is why we do not see it. Health is great at the “Sara Lee” model, layer upon layer but no cream on top.
– Yes, IF they are linked well to other services. We ran a VED and showed that many patients could be served in other ways without an ED, however, they need an alternative e.g. a nurse to go out, a physio etc. Provided it is connected well to provide this, I’m for it. Without that it does not have as good value.
– Each area has it’s own population challenges which differ from others, for example aged populations, indigenous, cultural, religious, demographic etc. it is not a one state fits all scenario. Governance yes but not operational