The final quarter of the year in digital health in Australia featured three of the biggest stories of the year: the cyberattack on Medibank’s systems that saw sensitive health claims data released, the big bang go-live of ACT Health’s ambitious Epic-powered Digital Health Record, and the extraordinary news that NSW Health plans to rip out its hugely expensive Cerner eMR and replace it with Epic in what industry experts believe will be a billion-dollar endeavour.
There was some welcome movement on healthcare standards, with the Australian Digital Health Agency and HL7 partnering up and a national healthcare interoperability plan in the works; some progress with new Provider Connect Australia (PCA) service; and progress with ADHA’s Health API Gateway replacement program, which will see the critical business-to-business bundle of APIs that interact with clinical software upgraded to a modern, web services- and FHIR-based platform.
It wasn’t a great year for the Digital Health Cooperative Research Centre (DHCRC), which was launched with much fanfare and a lot of money in 2018 but has struggled since then to produce many achievements. It has gone through three different CEOs, all of whom left abruptly and with little explanation, until it settled on Research Australia chair Annette Schmiede earlier this year. There have been some wins, including the well-received Aged Care Data Compare project and one that is developing a new tool to improve medication selection and dosing for patients with poor kidney function that can be integrated with prescribing and dispensing software, but some projects seem to be repeats of other research over the years.
The decision-making process for funding has also been called into question, with one well-resourced bid looking at the use of artificial intelligence for addressing otitis media in Indigenous children receiving all the right marks but being cancelled at the final hurdle, seemingly on a whim. The DHCRC has subsequently invested in several other notable projects but with its seven-year funding envelope coming to an end in the next couple of years, it will need to put some runs on the board to justify the expenditure.
In primary care, a report into the $84.7 million Health Care Homes trial showed that there should be concerns about the Department of Health and Aged Care’s voluntary patient enrolment (VPE) plans, with the trial showing some improvements in patient access and chronic disease management processes, but no significant change in patient experience or health outcomes. The lead investigators were not able to reach a conclusion about the value for money of the program but that it did have ramifications for voluntary enrolment with general practices, along with bundled payments, primary care IT and processes to support practice transformation and shared care planning.
The IT problems were a feature. They were asked to use electronic shared care planning tools to give authorised health professionals and patients access to up-to-date electronic medical records, and a risk stratification tool (RST) embedded in practice management software to help find suitable patients. However, despite practices being paid a one-off grant of $10,000, many practices said it was insufficient to cover the costs of IT set-up and ongoing licensing and maintenance costs. The evaluation found that the My Health Record was increasingly useful for sharing information about HCH patients with external providers but shared care software was deemed not yet fit-for purpose.
The healthcare standards community got a bit of a boost towards the end of the year with the Australian Digital Health Agency (ADHA) signing a memorandum of understanding with HL7 Australia to support the development and implementation of digital health standards and specifications to help improve connectivity across the national healthcare system. HL7 has gone it alone on standards for a number of years since a breakdown in relations with ADHA’s predecessor, the National eHealth Transition Authority (NEHTA), along with the end of funding for eHealth standards development by the Department of Health. However, the MOU will see ADHA and HL7 work together, particularly Fast Healthcare Interoperability Resources (FHIR), along with training, education and uplift activities to support the health workforce to use the new standards.
ADHA said it hopes to release a national healthcare interoperability plan focusing on five focus areas to bring together the healthcare sector over the next five years. It also plans to release a standards catalogue to provide a one-stop shop for anybody interested in digital health standards, and is working to re-establish its relationship with Standards Australia and the wider healthcare standards community following a number of years of estrangement. A dedicated section of the agency has been working on a discrete program of work to rebuild relationships with standards development organisations, including HL7. The plan is to bring together the entire healthcare sector, including software vendors, providers of care, health service managers and government in a concerted and dedicated push over the next five years to bring about a much more connected healthcare system.
A notable feature of 2022 was the roll out of electronic prescriptions in the acute care sector as well as in primary care. In August, ADHA announced that Royal Perth Hospital was the first public hospital in the country to enable electronic prescriptions to be sent by SMS or email to community pharmacies. This is quite a complex undertaking as we found out in a terrific interview we did with WA Health’s Health Support Services (HSS) and Royal Perth. Hospital patients often have complex prescriptions on discharge, and one of the real successes of this project is the ability to not only produce an electronic token for one prescribed drug, but to also produce a paper script for another, and to allow patients to collect one medicine from the hospital pharmacy and the other when they are discharged back into the community.
The Australasian Institute of Digital Health held its 2022 Summit in Sydney in October in association with eHealth NSW. The institute announced that it had set up three new expert advisory groups to help inform opinion and policy in digital health, with former NSW Health director-general and Telstra Health managing director Mary Foley chairing a group looking at changing the business models of healthcare; former Department of Health deputy secretary and Health Workforce Australia head Mark Cormack chairing another group looking at advancing the digital health workforce; and well-known health security standards expert Trish Williams chairing the final group, which is looking at building trust and confidence in health and data.
An interesting development was the announcement by eHealth NSW and the NSW Agency for Clinical Innovation (ACI) that they were working together on a pilot of the state’s Health Outcomes and Patient Experience (HOPE) patient reported measures (PRMs) platform in early adopter sites in the primary care sector. A pilot in up to 30 general practices across three primary health networks (PHNs) is underway, allowing service providers and GPs to access HOPE using secure NSW Health credentials. The hope is then to integrate the platform into general practice software in a future phase of the project. Plans are also underway to integrate the platform with hospital-based patient administration systems (PAS) and the electronic medical record (eMR) from February next year.
The Australian Digital Health Agency’s new Provider Connect Australia (PCA) service went live with a select number of healthcare organisations across the country on November 1, as part of the initial phase of real world testing. It will now be tested by about 600 different sites, covering the gamut of small and large healthcare organisations across metro, rural and remote areas. The technology has been built using FHIR with APIs on both the publishing and business partner ends, and will support integration with practice management and clinical information systems.
Progress has also been made by ADHA on its mammoth national health infrastructure re-platforming program, with the third tranche of application programming interfaces in its Health API Gateway replacement program released. This will see the critical business-to-business bundle of APIs that interact with clinical software upgraded to a modern, web services- and FHIR-based platform. The work has been supported by Deloitte in a $20 million work program to replace the legacy Oracle API gateway that has underpinned the My Health Record system for over a decade. It has also been expanded to provide a platform for health information exchange across the broader health digital ecosystem, not just the MyHR, and follows a strategic move to the secure public cloud in July.
In late October, the big news broke that health insurer Medibank had been hacked, affecting its ahm and international student policy arms. While it was cagey at first, Medibank subsequently confirmed that the attack had in fact resulted in data being stolen – including codes for diagnoses and procedures – despite earlier hopes that it had failed. The news just kept getting worse, with the cyberattack not just affecting Medibank’s small ahm brand and international student business but its core Medibank business, which covers over four million customers. More data than thought was stolen, including “significant” amounts of health claims data.
In November, Medibank announced it would not pay a ransom to the hackers, saying there is only a limited chance that paying a ransom would ensure the data was returned. The numbers affected kept growing in what has turned out to be one of Australia’s worst cyber incidents, in which 9.7m customers may be affected. The hackers soon set to work releasing data on the dark web. The hackers then made their final data dump in December as they realised they were not going to get their money.
Also in November, ACT Health went live with its big bang implementation of the Epic-powered Digital Health Record. ACT Health CIO Peter O’Halloran, who led the mammoth project, said it was delivered through an “amazing collaboration” across the ACT public health system in conjunction with healthcare consumers and vendor partners including Epic, NTT and the ACT’s digital, data and technology solutions (DDTS) group. He described the implementation as the most complex and far-reaching implementation of Epic’s system in the Asia-Pacific region, including 11 modules that are being implemented in Australia for the first time, including patient administration, pathology and radiology. “This, combined with the exceptional clinicians in the ACT public health system will enable the ACT to quickly become the most digitally enabled healthcare system in Australia,” he said.
It was a huge achievement by ACT Health, which first released a tender for the DHR in 2019. It envisioned a sweeping change to digital health in the territory, requiring full electronic medical record capabilities, integration with medical devices and consumer health monitoring devices and a new patient administration system. ACT Health said it was aiming to achieve HIMSS Level 6 for the new system by 2023-24 and Level 7 by 2026-27. The tender was awarded to Epic in July 2020, with hopes it would be operational by 2022-23.
The COVID pandemic provided an opportunity to take a look at the system up close, with a full version going live in early 2021 to help manage COVID-19 vaccinations for the ACT public health system. The MyDHR consumer app, using Epic’s MyChart patient portal, was also configured and launched early to assist with appointment bookings. As the new system settles in, ACT Health is now running a small pilot of the DHR Link portal into the DHR that will allow general practices to access their patients’ medical records from Canberra Health Services and Calvary Public Hospital Bruce, with the patient’s consent.
But just as ACT Health was basking in the limelight for its achievement, NSW Health swooped in with a massive shake-up of the health IT sector in Australia, announcing that it would replace the Cerner EMR it has been using and building upon for almost two decades with the Epic system under its Single Digital Patient Record (SDPR) plan.
Not only will Cerner and the Orion Health EMRs be replaced with Epic’s offering, but so will the five pathology systems and the several patient administration system instances. NSW Health also plans to replace some other clinical systems, although it is refusing to identify which ones. We estimate that the full cost of the plan over 10 years will approach if not exceed $1 billion. eHealth NSW insists that it has secured the funding. The announcement was Pulse+IT’s most-read story for the year, and for many years. We’ll watch with interest as it rolls out.
Primary care
Two Australian medical colleges are working together to run a pilot of the UK’s Royal College of Radiologists iRefer diagnostic imaging guidelines. The Royal Australian and New Zealand College of Radiologists (RANZCR) has an exclusive license for iRefer in Australia and New Zealand and is set to run a pilot with the Royal Australian College of General Practitioners (RACGP) to see if it can be used as an integrated clinical decision support tool in general practice. The guidelines are aimed at helping clinicians to determine the most appropriate imaging procedures for a range of clinical problems.
GPs in South Australia and Western Australia now have free access to the SR Specialists & Referrals eReferral service, joining Victoria, Tasmania, NSW and the ACT. SR Specialists & Referrals is the online version of Cervin Media’s Medical Specialists Directory and is integrated with HealthLink’s SmartForm technology. Users of the Best Practice, MedicalDirector and Genie practice management systems can send eReferrals via HealthLink, which is integrated into all three systems, with the option of using a portal if needed.
Sydney’s CMH Practice Management signed up to offer its Clinimetrix medical intelligence platform to practices using audit, tax and consulting services firm RSM Australia’s professional services. CMH has developed Clinimetrix as an analytics tool that combines both financial and clinical metrics to help medical practices manage risk and generate more income. Clinimetrix is part of Best Practice Software’s partner network, integrating with BP’s clinical and financial capabilities.
Healthdirect Australia’s National Coronavirus Helpline secure messaging service for COVID-19 antiviral treatment eligibility sent more than 20,000 notifications to GPs and GP respiratory clinics since it began in NSW in May. The service is using existing secure messaging systems as well as an innovative solution jointly designed and built by Telstra Health that uses Microsoft Azure cloud services and Lyniate’s Rhapsody middleware to integrate Healthdirect’s CRM with each of the messaging networks through standards-based APIs and HL7 messaging.
Specialist medical software market leader Genie Solutions has released an integrated dictation solution app called Voice, developed in association with Nuance Communications, to enable specialists to dictate letters directly from their mobile phone. The app is available for iOS and Android users of Genie Solutions’ Gentu cloud-based practice management system and is one of a number of new applications being developed for Genie’s cloud marketplace platform.
Acute care
Telstra Health and joint venture partner PowerHealth launched a new analytics and benchmarking solution for public and private hospitals called PowerAnalytics, which went live at its first implementation at the Central Coast Local Health District in NSW. The PowerAnalytics digital health solution uses PowerHealth’s existing PowerPerformance Manager (PPM) and Telstra Health’s Kyra Flow in a solution the partners say can offer ‘actionable insights’ across operational and financial performance in healthcare. PPM is described as a web-based system that calculates hospital service delivery costs, integrating private and public funding revenue, while Kyra Flow, part of Telstra Health’s Kyra suite of hospital solutions, provides a single view of patient flow information, drawing from inpatient, elective, emergency and other compatible hospital systems.
Healthcare software solutions giant Dedalus introduced the Swiftqueue enterprise appointment and scheduling platform for healthcare to the Australian and New Zealand market this year, offering management of referrals, waiting lists and clinical appointments across acute and community services. Dedalus acquired the Irish-headquartered Swiftqueue in 2021, adding it to the company’s existing scheduling and appointment handling capabilities. The technology is used by hospitals and clinics across the UK’s NHS and Ireland’s HSE, as well as in Canada. Dedalus describes the solution as enabling patients and citizens to access healthcare services from hospitals, clinics and specialists through a digital front door. This includes a portal where patients can view, reschedule, cancel appointments and view specific results.
Sydney’s Macquarie University Hospital is rolling out Prospitalia h-trak’s supply chain management solution in all interventional departments of the hospital, including operating theatres, angio suite, and the endoscopy and trans-oesophageal echocardiogram (TOE) departments. The h-trak system includes a comprehensive database of medical and surgical products and prostheses, as well as a surgical preference card management system that are integrated to the hospital’s inventory management and billing systems. This allows for automatic and accurate billing, purchasing and cost reporting management, with point of care data capture using mobile technology.
Citadel Health’s Charm oncology information management solution became the first to integrate with the My Health Record system, enabling specialists to upload a range of My Health Record documents as part of the existing clinical workflow. This includes a chemotherapy event summary when the treatment day is completed in Charm, a prescription record when using Charm’s scriptwriter module and specialist letters from the Charm’s document manager.
Aged care
The groundbreaking Aged Care Data Compare (ACDC) project is about to go into its third phase, bringing together a number of elements that are set to revolutionise the collection, measurement and analysis of aged care data in Australia. Along with an inventory of standardised data items and a library of quality indicators, the project has also developed a prototype data analysis system that uses the University of Queensland’s QRIS platform, an analytics FHIR server called Pathling, a secure eResearch platform called SeRP, and a clinical data repository and integration platform using FHIR called Smile CDR. The third phase will bring together the three main components developed in the early stages of the project and will be implemented and operationalised in collaboration with a large aged care provider. It is also being trialled with a major software provider.
One trial that didn’t go too well was SA Health’s trial of CCTV to detect falls and other incidents in the residential aged care setting. An evaluation of the trial found that too many false alerts and a lack of accuracy in artificial intelligence technology meant CCTV was not yet at a mature enough stage to be useful. SA Health contracted PricewaterhouseCoopers to evaluate the acceptability and viability of using surveillance and monitoring within residential care as part of its 12-month CCTV project in two facilities over the last year. The trial got underway in April 2021 using an artificial intelligence-enabled audio-visual surveillance and monitoring system developed by local electronic security solutions firm Sturdie Trade Services, which can detect falls, calls for help and one- and two-way violence.
The trial – co-funded by the Commonwealth and state governments for $785,000 – was also plagued by delays. It was originally expected to get underway in 2019 but was delayed first by the withdrawal of its original technology partner, UK-headquartered CCTV in aged care specialist Care Protect, and then by the COVID-19 pandemic. AV surveillance was installed in common areas and resident bedrooms at both sites, with cameras and sound devices in bedrooms switched on with resident consent. While the evaluation found it was accepted and supported by residents and their families, the AI technology had a high rate of alerts and was not yet sufficiently accurate at detecting incidents in a residential aged care setting and wasn’t acceptable to staff.
SA Health is expanding its $10 million Virtual Care Service to more than 150 residential aged care facilities in the state, following a pilot in 11 Eldercare facilities. The service will enable aged care staff and first responders to have direct access to emergency medical and nursing staff and clinical advice by video link consultations to assess, monitor and determine care options. Aged care facilities are now also being provided access to the service, using tablet computers that links them with clinical teams including emergency physicians, general medicine, general practice, pharmacy and nursing clinicians.
Pharmacy
Dedalus is planning to introduce a new robotic oncology compounding system to the Australian and New Zealand markets, aimed at automating the preparation of oncology medications while also integrating with EMRs and specialist oncology prescribing, dispensing and compounding software. Pharmoduct is a TGA- and Medsafe-approved solution for the sterile preparation of personalised antineoplastic drugs that is also able to integrate with software solutions, promising to improve order accuracy, speed and scheduling of compounding orders. Dedalus says the solution aims to speed up personalised chemotherapy compounding while also making it safer for compounding and drug administration staff.
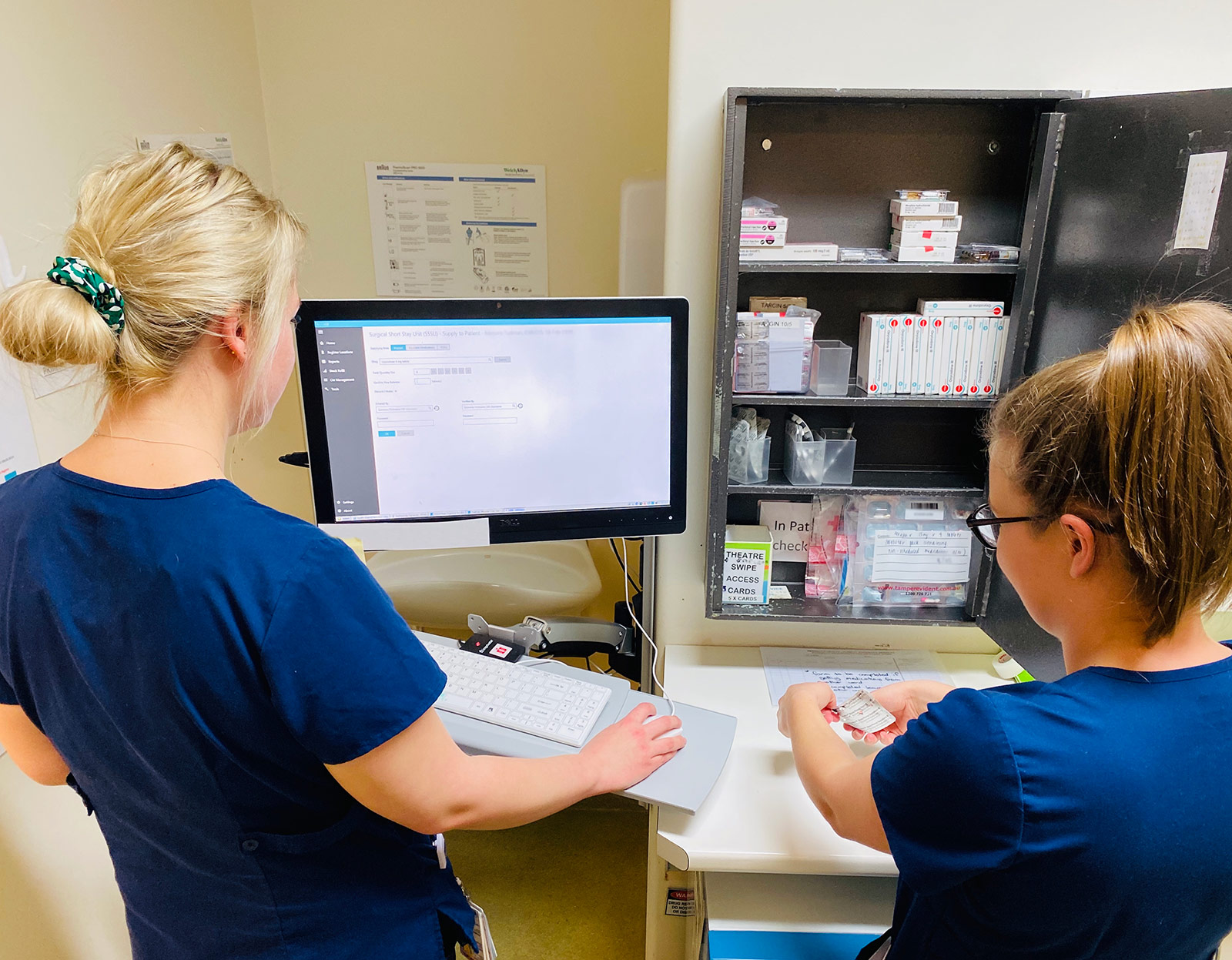
Healthcare software company Modeus won a contract with the shared services centre for WA’s public health services and hospitals, Health Support Services, to roll out its HS8 controlled medication register application across the WA hospital network. HS8 is a medication management software platform (pictured) that enables paperless controlled drug administration in all areas of a hospital including pharmacies, wards and theatres. It is integrated with other hospital software systems, including iPharmacy, patient administration systems (PAS) and Active Directory, removing duplication and making workflows quicker and more accurate.
Some of the more interesting software, apps and new players in the market that caught our eye this year included:
- Telehealth platform My Emergency Doctor won a contract with Ambulance Tasmania to provide telehealth consultation services as part of its secondary triage project. Ambulance Tasmania issued a tender for a new secondary triage clinical decision support system in 2019 to help reduce growth in demand for ambulance services for conditions better managed by primary care.
- Aged and disability care management software vendor Lumary partnered with care communication platform Hayylo to offer an integrated digital solution. Lumary markets a care management software platform to help aged care providers deliver care at home to older people receiving funded programs, while Hayylo’s communication platform promises to streamline communications through branded apps, SMS, email and voice channels. The company has a similar integration with Telstra Health’s care management system.
- Sydney’s Westmead Hospital is piloting a sepsis risk tool in its emergency department waiting room to try to enhance the detection of sepsis while patients are still waiting for care. A range of NSW Health partners have worked together to develop the clinical decision support tool, which collects demographic and vital signs data being entered into the hospital’s EMR and applies an algorithm to flag patients most at risk of sepsis. If the data shows an increase in the number of sepsis cases identified, eHealth NSW will explore scaling the solution statewide.
- Medical imaging and report sharing solution vendor Zed Technologies integrated clinical communication specialist Foxo’s Guest Chat module into its web viewer, aiming to improve communication between primary care specialists and diagnostic imaging providers. Guest Chat allows any Foxo-enabled organisation to share or embed a URL into reports, results and referrals and provide a secure and live communication thread that opens up a live chat between clinical or clerical teams and referrers.
- Australian health tech company TeleMedC’s RetinoScan technology is set to be trialled in two rural primary care sites in Western Australia and NSW to try to improve access to eye health screenings and reduce the incidence of preventable blindness. RetinoScan can help detect diabetic eye disease, glaucoma and age-related macular degeneration by capturing an image of the retina and using machine learning to produce a diagnosis within a matter of minutes. It is also being rolled out to general practices in both rural and metropolitan regions, as well as trials for use in the hospital sector and even in shopping centre kiosks.